
Dr. Mel Vincent, Director of Psychiatric Services
An insight into the Opioid crisis from a Treatment Center Director
Dr. Vincent’s journey through medicine and eventually to his specialty can be seen as elaborate but tortuous, not too dissimilar to that of today’s drug and addiction crises.
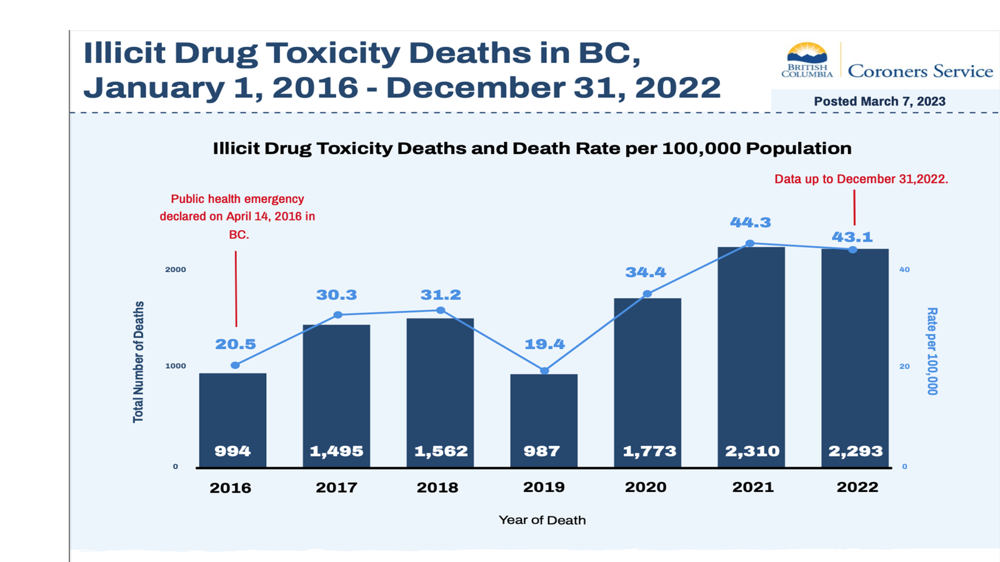
In an election year, this topic resonates soundly in all of today’s media as well as having severe impacts on the family members and the communities trying to deal with this overburdening reality. As seen in the data from BC’s Coroner Service, the Province witnessed a 50 % uptick in the rate of mortality per 100,000 of the population from 20.5 in 2016 when a public health emergency was declared, and an increase of 50 % the following year, with a certain leveling off subsequently but now to 2-fold 2016 figures, as 2022 figures reveal.
 The Province moved to towards a decriminalization model, with expansion of harm reduction strategies in an attempt to get a control on the crisis. The problem is very complex however, and we sit at the intersection of an increasing number of unhoused people exhibiting mental disorders and addiction, as well as an overwhelmed medical system, that is unable to provide the special services needed let alone addressing basic health needs of its ordinary citizens, and city cores struggling with methods to address the unruliness, and decay of their streets and the effects on local business.
The Province moved to towards a decriminalization model, with expansion of harm reduction strategies in an attempt to get a control on the crisis. The problem is very complex however, and we sit at the intersection of an increasing number of unhoused people exhibiting mental disorders and addiction, as well as an overwhelmed medical system, that is unable to provide the special services needed let alone addressing basic health needs of its ordinary citizens, and city cores struggling with methods to address the unruliness, and decay of their streets and the effects on local business.
The physiological reasons of addiction as explained, are rooted in our brain’s reward center, and have an evolutionary significance. Unfortunately, the substances that give the biggest highs for users also are for the most part very addictive. Dr. Vincent also highlighted the evolution of treatment facilities and their personnel and that the early staff were often recovering addicts themselves and the specialty had not evolved until medical education tackled it much later in their programs. Now, he felt, better trained specialists were involved within specialized treatment programs such as the private institution Homewood in Nanaimo, part of a chain similar US to based corporate models.
The evolution of substance use began in the early days of colonization, when the British Empire’s trading with China hit roadblocks, whereupon its trading partner refused to make payments of goods in silver, hoarding it, instead. The solution for Britain was to trade with opium, whereupon the worker population became hooked and spent much of their time in the infamous opium dens. In the 1960’s much of drug us was centered on so-called soft drugs, but with a small core of individuals experimenting with the hard-core ones such as LSD. The 70’s brought in the era of amphetamines and they became much more mainstream than previous substances. Cocaine also soon became the drug of choice in the socializing upper income crowds later but also revealed its presence on the streets and cheaper varieties using crack cocaine became available.
There was nothing to match anything of mainstream use however, as the introduction of a potent substance from an unsuspecting and duped provider as the medical establishment itself. Pain management became a model within the schools and adopted in hospitals for patients either of trauma related visits or surgery, thus, an alternative to these potent elixirs used in hospitals, when offered to the more general medicine practitioners, such as of family medicine was quickly adopted. This rapid adoption by GP’s brought about by an unscrupulous company with a primed and dedicated sales force that knew no bounds, was only precipitated because of the false allegations and statements of this company assuring OxyContin had no addiction issues. The sociological effects were horrific as now, the system was absorbing a much more mainstay crowd and many became embroiled in a drug-world they, would never have suspected was to be their future, as well as their families.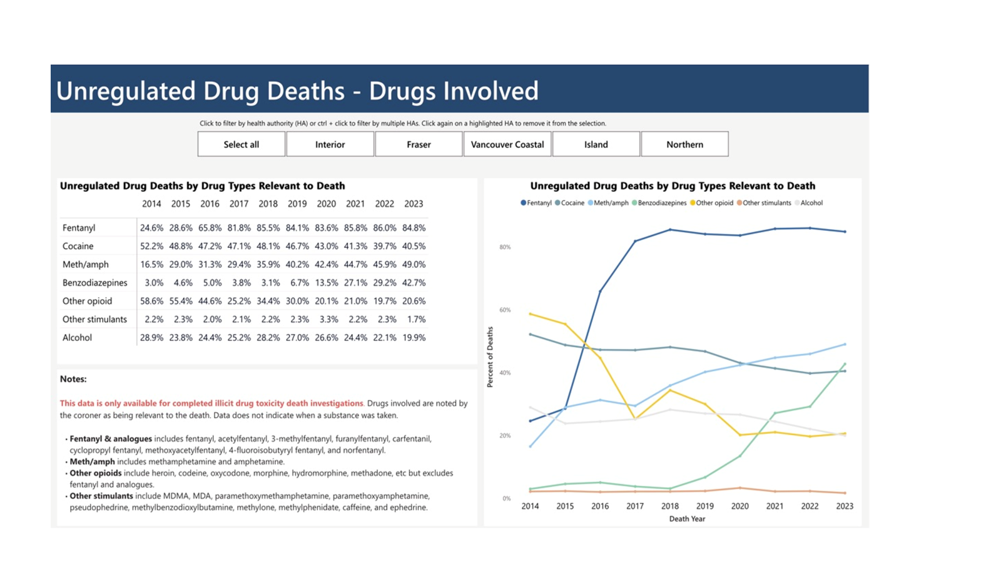
Dr. Vincent itemized the approach towards harm reduction, and the steps towards its more, lofty goals of encompassing a fully integrated approach, only requiring large inputs of capital from government in order to achieve a rehabilitation process within an integrated model with possibility of larger scale treatments centers that would entail the use of government buildings that are being underused which could be ramped up quicker than a full scale new-build plan. Private treatment centers would still exist and provide relief in numbers to a system that is under enormous pressure at the moment.

Various treatment modalities were featured and a foresight to a worse problem appearing on the streets, being the incorporation not only of fentanyl but of benzodiazepams, which also have a negative effect on our breathing centre, but unlike fentanyl these effects are not reversible even when intervened early as they have no source of reversal because there are no pharmacological solutions here.
In addition, Dr. Vincent highlighted another toxic drug with which we are probably all familiar with, but have not received enough signaling with regards to its potent nefarious effects beyond simple addiction, but as factor in many diseases which we are also familiar with, including, cancers of the breast, colon, liver and esophagus, and heart disease and stroke. It is with this background that Health Canada’s new guidelines seem radically different from previous ones, with a guide of a maximum of 2 drinks per week, to avoid all repercussions.
https://www.ccsa.ca/canadas-guidance-alcohol-and-health
report by
Marcel Lalonde


